ACLS
Advanced cardiovascular life support (ACLS) impacts multiple key links in the chain of survival that include interventions to prevent cardiac arrest, treat cardiac arrest, and improve outcomes of patients who achieve return of spontaneous circulation (ROSC) after cardiac arrest.
ACLS interventions aimed at preventing cardiac arrest include airway management, ventilation support, and treatment of bradyarrhythmias and tachyarrhythmias.
For the treatment of cardiac arrest, ACLS interventions build on the basic life support (BLS) foundation of immediate recognition and activation of the emergency response system, early CPR, and rapid defibrillation to further increase the likelihood of ROSC with drug therapy, advanced airway management, and physiologic monitoring.
Following ROSC, survival and neurologic outcome can be improved with integrated post–cardiac arrest care.
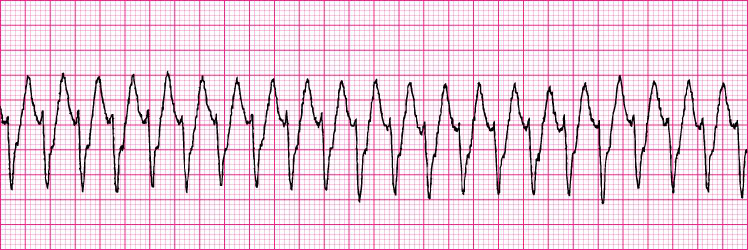
Ventricular Tachycardia
Key changes from the 2005 ACLS Guidelines include:
- Continuous quantitative waveform capnography is recommended for confirmation and monitoring of endotracheal tube placement.
- Cardiac arrest algorithms are simplified and redesigned to emphasize the importance of high-quality CPR (including chest compressions of adequate rate and depth, allowing complete chest recoil after each compression, minimizing interruptions in chest compressions and avoiding excessive ventilation).
- Atropine is no longer recommended for routine use in the management of pulseless electrical activity (PEA)/asystole.
- There is an increased emphasis on physiologic monitoring to optimize CPR quality and detect ROSC.
- Chronotropic drug infusions are recommended as an alternative to pacing in symptomatic and unstable bradycardia.
-
Adenosine is recommended as a safe and potentially effective therapy in the initial management of stable undifferentiated regular monomorphic wide-complex tachycardia.
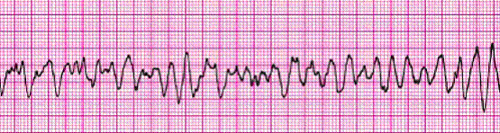
Ventricular Fibrillation






